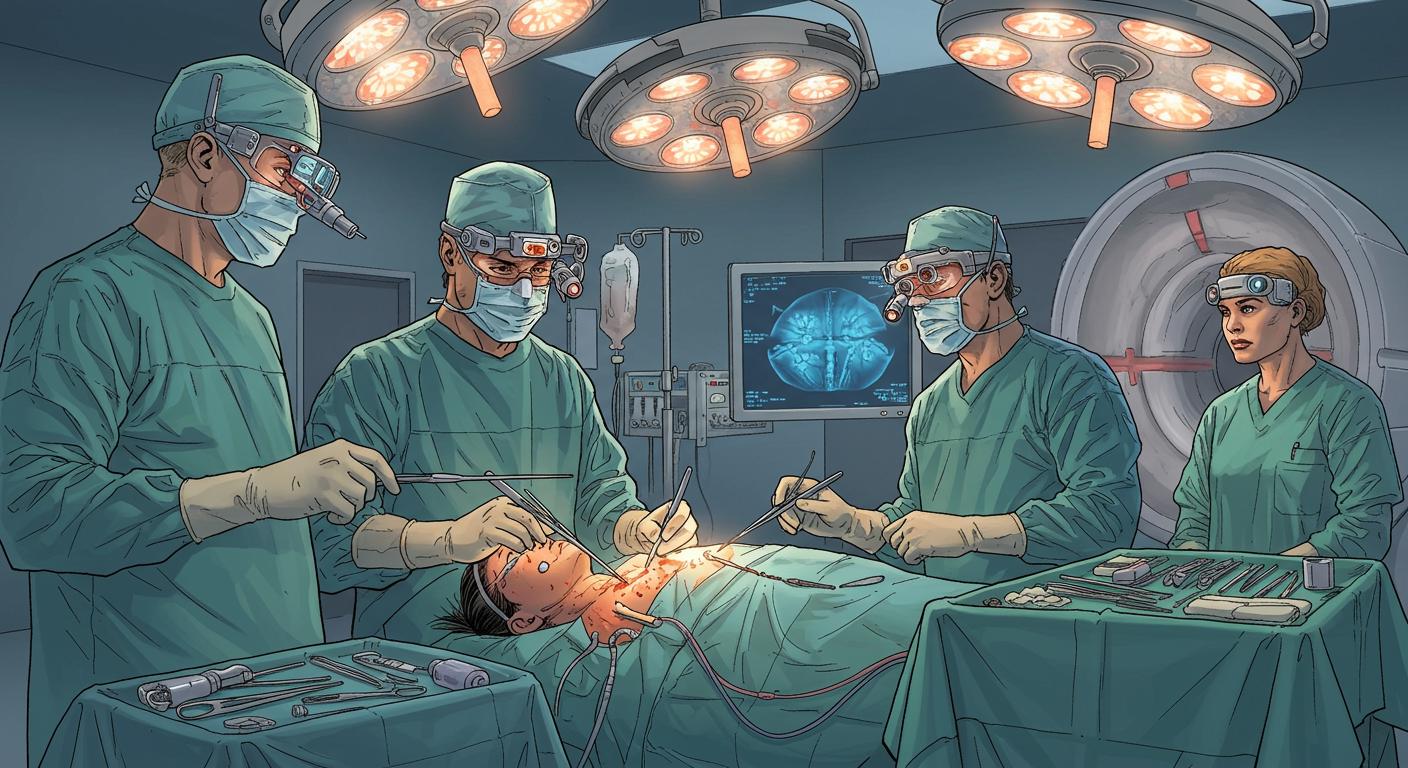
Medicine is replete with stories where perseverance meets pure chance, but every now and then, a case comes along so circuitous—and let’s be honest, eyebrow-raising—that it could make even a seasoned archivist check their notes twice. The saga of Karla Flores and her University of Maryland Medical Center surgical team, as detailed by CBS News, fits firmly in that category: what began as persistent double vision led to the medical equivalent of a wrong turn, revealing not just one, but two exceptionally rare tumors and culminating in a surgical approach that would make most anatomy textbooks do a double-take.
The Accidental Oversight: When Mistakes Are Fortuitous
Karla Flores’s health odyssey started at 18 with double vision and mounting uncertainty. Efforts to pin down a cause went nowhere until an ophthalmologist referred her to a neurosurgeon, setting off a chain of events most would only expect to encounter in the odder corners of a medical library. According to information cited by CBS News, imaging eventually pointed to a diagnosis few clinicians ever make in their careers: a chordoma nestled precariously around her brain stem. Reports from the Cleveland Clinic, referenced in the article, underscore the rarity—roughly 300 cases occur yearly nationwide.
Then, technology’s fickle hand intervened. When Flores was being prepped for surgery, the MRI technician—presumably through a minor lapse or a simple slip of hand—positioned the scan a tad lower than intended. This unintended angle, the outlet notes, inadvertently captured a second tumor at the top of Flores’s spine. Here, the tumor’s placement was particularly menacing: it wrapped around her spinal cord and invaded her vertebrae—terrain so fraught that missing it, as the reporting highlights, may well have left her paralyzed.
How many times do life-altering revelations depend on such split-second misalignments? Can the happiest medical accidents ever truly be planned?
Charting a Surgical Path Where None Existed
With two tumors identified, the standard playbook quickly ran out of pages. CBS News relates that in conventional practice, surgeons would access a spinal tumor from behind. Unfortunately, this chordoma’s hideout—tucked at the front of Flores’s spinal cord—ruled that out. The idea of approaching via the nose, previously used in her first brain stem surgery, offered too little room for maneuver.
Insights shared by Dr. Mohamed Labib, the lead neurosurgeon on the case, paint an unsettling picture of the options discussed. One colleague, as described earlier in the report, bluntly suggested shifting focus to palliative care. Labib, however, remained unconvinced that Flores’s prognosis should be written off so quickly. CBS News documents how Labib’s insistence on seeking unconventional solutions drew the team back to the dozens of scanned images and lab simulations, determined to sidestep resigned fatalism.
Through the Eyeball: The “Third Nostril” Solution
Labib and colleagues set to work on an idea that straddled the boundaries of ingenuity and anatomical audacity. Drawing inspiration from earlier experience operating near the orbit—though never for a spinal tumor—they conceived what’s since been dubbed the “third nostril” approach. Instead of moving through the familiar routes, the plan would see surgeons entering through the lower eyelid, removing bone from the eye socket and cheek, and then tunneling directly to the spinal target.
Practicing for weeks on cadaver heads and skull models, as the outlet details, the surgical team sought to iron out each wrinkle. They needed to expand certain surgical tools and develop techniques to protect vital structures, all while keeping Flores’s external appearance untouched. Dr. Kalpesh T. Vakharia, described in the report as a facial plastic and reconstructive surgeon, began by accessing the area through the inner side of the lower eyelid, excising part of the eye socket and cheekbone. This gave space for Labib and Dr. Andrea Hebert (head and neck surgeon) to carefully drill down to the vertebral tumor, working painstakingly to remove it in a marathon effort that, according to team accounts, ran upward of 20 hours.
One almost wants to ask: is this resourcefulness born of desperation, or do truly novel solutions need a wall to run into first?
Recovery and the Cost of Medical Innovation
The team’s efforts yielded a textbook-perfect outcome—at least surgically. Flores emerged tumor-free, her eye socket rebuilt with titanium, her cheek with bone from her hip, and, despite the magnitude of the undertaking, she was left with no visible scars. Still, as CBS News emphasizes, her journey is far from over. Lingering nerve damage hampers movement in her left eye, though ongoing physical therapy offers hope.
There’s no ignoring the collateral challenges either. The article further notes that Flores is now wrestling with medical bills totaling around $600,000, while her GoFundMe has raised only a fraction of that total. Between periodic checkups at the medical center and the grind of rehabilitative therapy, her determination remains, but the financial strain endures.
CBS News relays Flores’s own reflections—she’s focusing on day-by-day progress and is considering training as a manicurist when her health stabilizes. The report also shares Labib’s belief that this “third nostril” method opens new avenues for treating otherwise unreachable tumors in the upper spine, and could, with refinement, become a new standard.
Charting New Territories (Through the Cheekbone, No Less)
Every now and again, a convergence of happenstance, determination, and creativity pushes medicine into uncharted territory. This entire episode serves as an improbable reminder: sometimes, technical mishaps can deliver more than a workaround—they reveal new frontiers.
One wonders how many other surgical innovations have emerged not from deliberate design, but from necessity or twist-of-fate error. Is it a question of being prepared for the unexpected, or just being willing to see opportunity when something goes awry? Either way, the spectacle of a tumor removed through the eye socket, with no external scars to show for it, feels almost absurd—until you realize it’s now part of someone’s lived reality.
And perhaps, for some corners of medicine (and life), the best route really does involve taking “the scenic way”—even if the scenery includes a brief, unlikely detour through the eyeball.