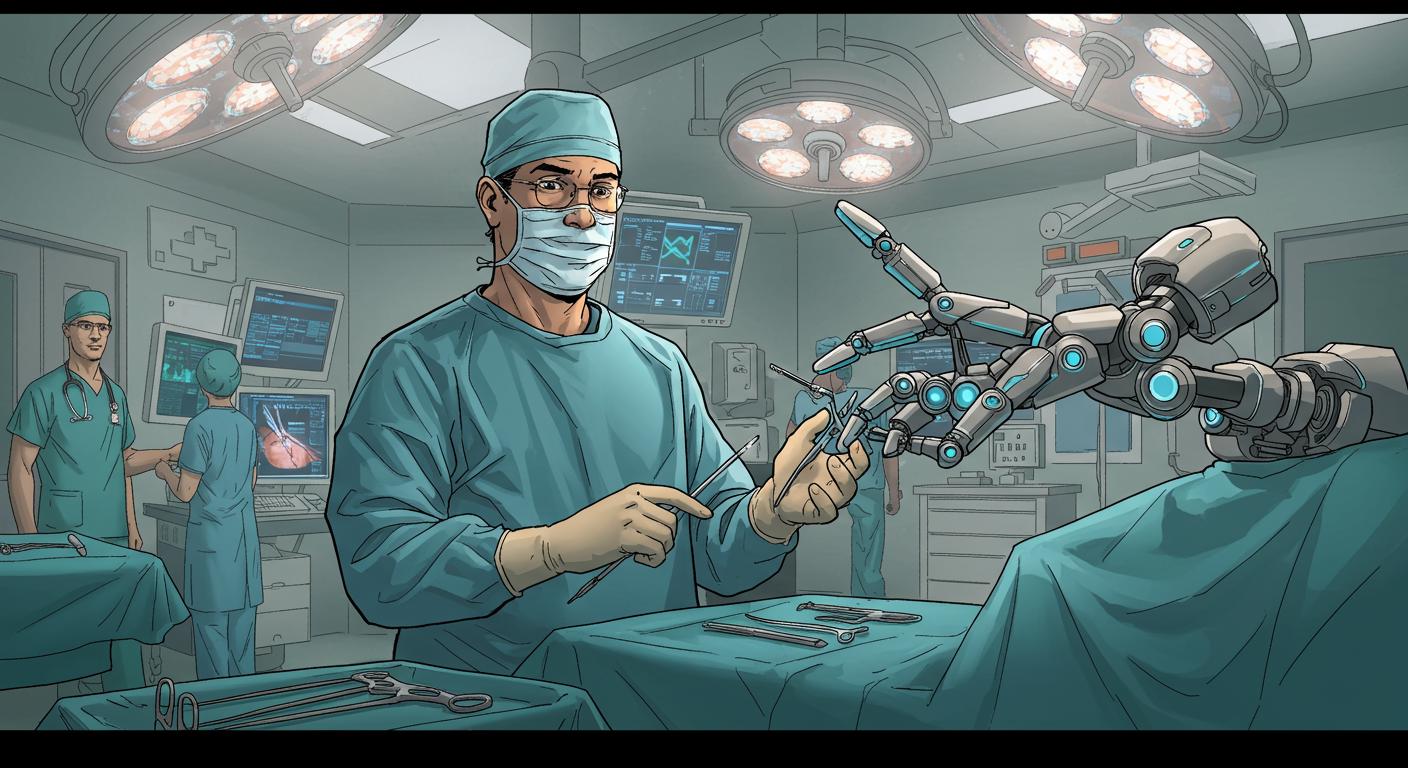
Picture this: You’re past forty-five, sitting in the muted blues of an exam room, when your urologist announces a new assistant will be handling your prostate check. In walks… a robotic finger. As detailed in a report by mauromar on Hiveblog, this isn’t a fever dream or the set-up to an unusually focused science fiction story. A research team at the University of Science and Technology of China (USTC) has introduced a highly flexible robotic finger, tailored specifically for medical examinations—especially those most men would rather not discuss over dinner.
High-Tech Dexterity Meets Age-Old Awkwardness
The prostate: small, walnut-shaped, vital, and, for those crossing into midlife, a critical watchpoint for cancer and other issues. Traditional exams, as summarized in the report, involve a urologist relying on their own sense of touch—direct, personal, and, for many, acutely uncomfortable.
This is where USTC’s invention enters, aiming to alleviate both diagnostic inconsistencies and social squeamishness. According to mauromar’s analysis, the robotic finger is engineered to replicate the fine motor skills of a human finger, yet with significant upgrades. The system boasts enhanced sensitivity and precision, allowing it to take a patient’s pulse, detect lumps, and presumably avoid any telltale sigh of resignation before getting to work. The original article points out that this could sharply reduce diagnostic errors; after all, robots don’t get distracted, tired, or second-guess their impressions.
The design, described in detail by mauromar, seeks to make such examinations less uncomfortable for patients. The robotic finger’s consistent diagnostic approach—never wavering, never taking a day off—could result in more streamlined and less anxiety-inducing appointments. For anyone who’s ever felt their dignity slip away during a checkup, the idea of being examined by a highly calibrated mechanism rather than a fellow human might come as a relief, or at minimum, a new flavor of discomfort.
The Why and the “Really?” of Robotic Exams
Clustered within the same report, several advantages surface. Increasing exam efficiency, reducing the backlog of patients, and enabling earlier detection of prostate cancer—the latter of which remains, per mauromar’s overview, one of the top health threats to men. Early detection is notoriously linked to better treatment outcomes, making any innovation on that front worthy of note (awkwardness aside).
There’s a peculiar double-edge to this development: many may find a robotic examiner less mortifying than a human one, especially given the societal reluctance to discuss prostate health in the first place. Would embarrassment wane in the presence of what is, essentially, a hyper-precise medical appliance? Or would the uncanny valley pop up in an unexpectedly personal context?
The report also suggests that with the human variable removed, the diagnostic process could be not only less embarrassing but more accurate. The idea of an unflappable, impartial examiner dispensing with niggling human error has its appeal—yet it raises practical questions. Can a programmable sensor truly replicate the nuanced pressure and intuition of a trained doctor? And in a world increasingly orchestrated by algorithms, when do we push back and say, “actually, I’d prefer the old-fashioned awkwardness, thanks”?
The Uncomfortable, Unromantic Path Toward Progress
As highlighted by mauromar, there’s no avoiding the statistics: prostate cancer is one of the most common forms of cancer in men, and catching it early is crucial. Reluctance to get screened—often rooted in discomfort—remains a persistent healthcare obstacle. If a robotic finger can sidestep some of these hesitations, even just by making the experience more bearable, the effect on public health could be quietly dramatic.
Additional coverage, such as Interesting Engineering’s analysis, emphasizes the design’s goal of marrying comfort with clinical accuracy. This isn’t about mad science for its own sake; it’s a pointed response to the sluggishness and inconsistency of traditional manual screening. Echoed by other outlets like Mundo Deportivo, the coming era could well include less waiting, more precise results, and an overall gentler approach to a topic most would rather sweep under the exam table.
Yet the existential oddity refuses to evaporate. Is there something undeniably bizarre about trusting one’s well-being to a “highly flexible robotic digit”? Very much so. Will routine acceptance settle in with time, making this the faintly comic grandparent tale of the future? Almost certainly. The report encapsulates the underlying irony: one of the least glamorous developments in med-tech may become among the most quietly impactful.
Stiff Competition for Awkwardness
Ultimately, what lingers is a mix of wry amusement and cautious optimism. The move to robotic assistance in prostate exams is about improving outcomes—reducing errors and, perhaps above all, trimming the embarrassment that keeps so many from getting checked in the first place. If the trade-off for better health is a little uncanny technological intervention in a deeply traditional ritual, is that so bad? Or will this be one advance that, after initial hesitation, becomes as routine and unremarkable as digital thermometers or self-checkout lines?
Prostate exams may never be a favorite topic, but with this blend of weird science and practical benefit, the future might just be a little less awkward—and if not, at least differently awkward. Would our ancestors have dreamed of a world where checkups required introducing yourself to a robot finger? Probably not. But in this strange, quietly hopeful chapter in medicine, progress sometimes comes one digit at a time.